Is ADHD Different for Men and Women?

Is ADHD really different for men and women? Not always.
Historically, ADHD has been studied through a predominantly ‘male’ lens, leading to a skewed perception of the disorder and fewer research insights around ADHD in women. We’ll take a deeper dive into what the research tells us and what we still don’t know.
Symptom Presentation
One of the fundamental distinctions between ADHD in women and men lies in the symptom presentation. Girls and women are less likely to present with hyperactive/impulsive symptoms of ADHD than boys and men, or when they do, these symptoms can show up later in development than boys (Murray et al., 2019). Women are also more likely to internalize their hyperactive/impulsive symptoms, influencing the manifestation of symptoms (Hinshaw et al., 2022). Women with ADHD also commonly experience a comorbid anxiety or depression disorder, making it difficult to disentangle ADHD symptoms (Young et al., 2020). Together, women are commonly underdiagnosed, misdiagnosed, or have symptoms attributed to another disorder.
Hormone and Brain Differences
ADHD diagnoses do not differ amongst sexes in later adulthood (Kok et al., 2020), highlighting that the difference in prevalence rates cannot be explained away by hormonal or neurobiological differences alone. That said, there are a handful of studies to suggest that there are some neurobiological differences of ADHD in males and females (Mahone, & Wodka, 2008). Studies also show that hormonal fluctuations in female’s lives, particularly during puberty (Murray et al., 2019), pregnancy, postpartum, and menopause (Kittel-Schneider et al., 2021), can influence how ADHD symptoms onset and present.
Treatment Implications
Overall, medication recommendations do not differ by sex (Young et al., 2020). However, due to the historically prominent focus of ADHD in males, medication and therapy studies have recruited samples with a male bias. That means less is known about the impacts and appropriate dosage of medication and therapy for women with ADHD. Females are less likely to be prescribed ADHD medication than males (Kok et al., 2020). There is some evidence that medications for ADHD may work differently in women due to hormonal fluctuations (Kok et al., 2020) and some data to suggest ADHD medication in women can lead to higher rates of eating disorders (Gibbs et al., 2006). Continued research with representative samples is needed before we fully know the answer to these questions. Addressing ADHD in women requires tailored treatment approaches, with special consideration on medication effects, dosage, and comorbid or secondary mental health disorders.
Final Thoughts
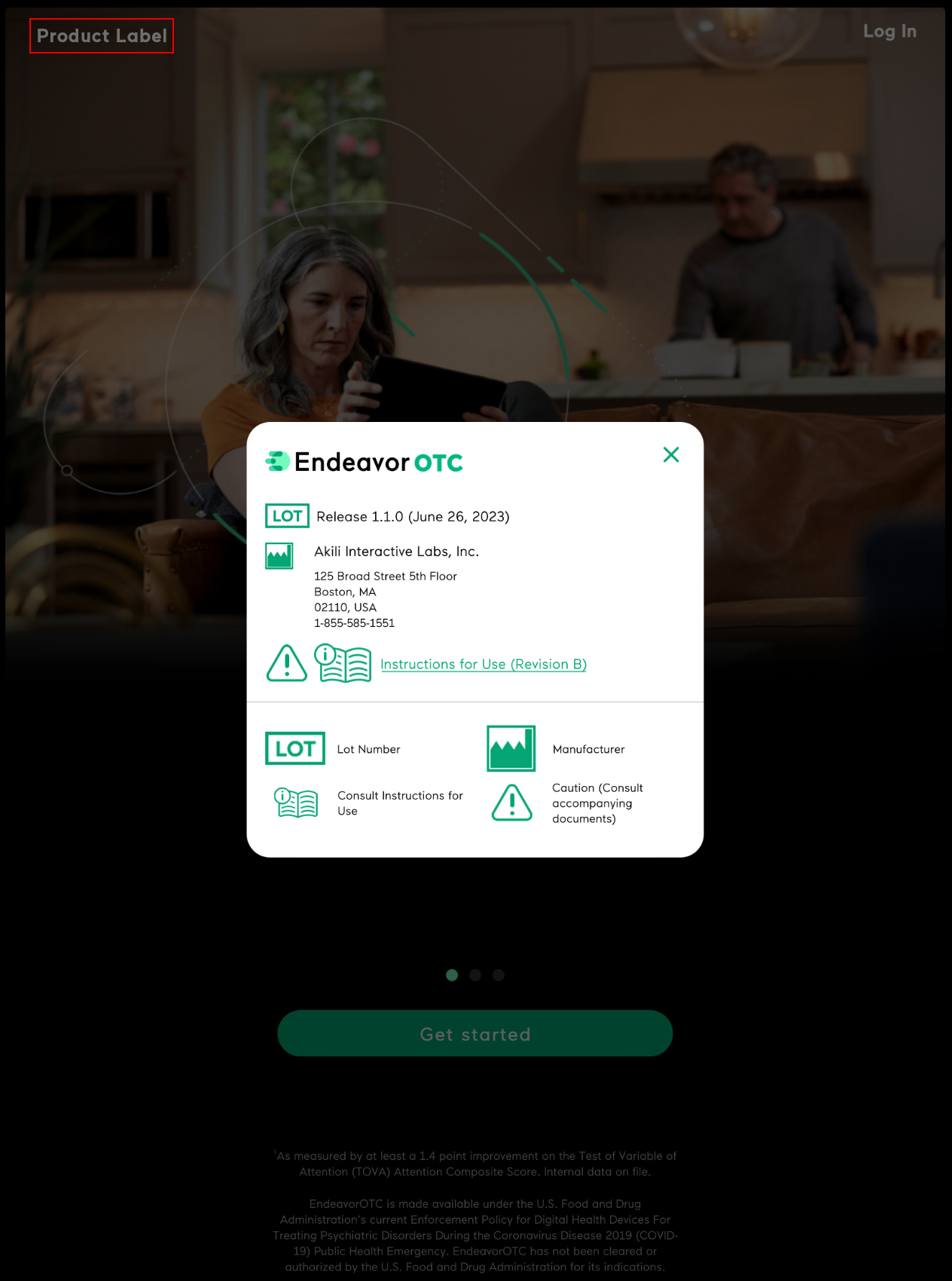
What we do know, is that it is important for women and their loved ones to be proactive in seeking an accurate evaluation when ADHD is suspected. Initiating conversations with healthcare providers and advocating for thorough assessment can help bridge the gap in understanding and ensure that women with ADHD receive the support and treatment they need to thrive. If you are interested in understanding the severity of your symptoms, please check out this free, online screening tool for ADHD. And for those that are diagnosed, finding the right management and treatment options that fit with their life is key. This may be medication, behavioral therapy, or some combination of the two—but for others, these options may not be the right ones or may not provide enough relief. EndeavorOTC offers an effective, safe non-drug option for improving ADHD-related symptoms and focus in adults. Please review more information on EndeavorOTC and talk to your healthcare provider to see if it might be right for you during this time.
Note, while this article predominantly discusses differences in terms of men and women, it is important to note that there are both sex and gender influences on ADHD presentation and treatment effects. Scientific papers vary on which term they use.
About the Author
-
Jessica E. Flannery, PhD is the Associate Director of Clinical Science at Akili. She is a clinical licensed psychologist, an ADHD-Certified Clinical Services Provider (ADHD-CCSP), and a developmental social neuroscientist. She has published over 50 peer-reviewed articles, received prestigious fellowships and awards and is a prior TEDx speaker.